Medicare Advantage plans overcharge, deny needed services. The impact of privatization.
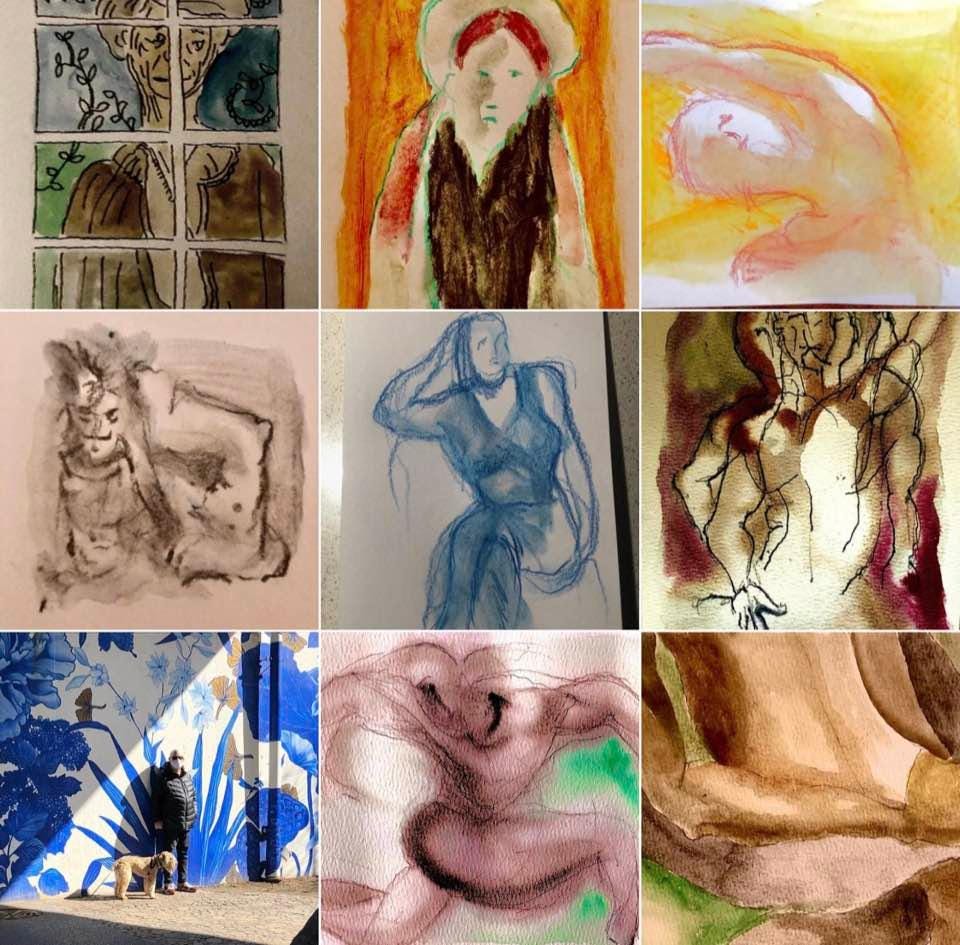
My art is all on Instagram @klonskyart.
For those of you not in Chicago the latest news is the Mayor Lori Lightfoot has all but officially announced she is running again and north side Congressman Mike Quigley, a fave of local political reporters, says he is not running.
In what must count as the strangest explanation for not running for an office, Quigley blamed his decision on the War in Ukraine.
And, of course, the need to spend time with his family.
If you have been following my posts you know I have been expressing great concern over the Biden administration’s plan to move everyone out of fee-for-service Medicare into a privatized Medicare Advantage-like system.
Our case file reviews determined that MAOs sometimes delayed or denied Medicare Advantage beneficiaries’ access to services, even though the requests met Medicare coverage rules. MAOs also denied payments to providers for some services that met both Medicare coverage rules and MAO billing rules. Denying requests that meet Medicare coverage rules may prevent or delay beneficiaries from receiving medically necessary care and can burden providers. Although some of the denials that
we reviewed were ultimately reversed by the MAOs, avoidable delays and extra steps create friction in the program and may create an administrative burden for beneficiaries, providers, and MAOs. Examples of health care services involved in denials that met Medicare coverage rules included advanced imaging services (e.g., MRIs) and stays in post- acute facilities (e.g., inpatient rehabilitation facilities).
Prior authorization requests. We found that among the prior authorization requests that MAOs denied, 13 percent met Medicare coverage rules—in other words, these services likely would have been approved for these beneficiaries under original Medicare (also known as Medicare fee-for-service). We identified two common causes of these denials. First, MAOs used clinical criteria that are not contained in Medicare coverage rules (e.g., requiring an x-ray before approving more advanced imaging), which led them to deny requests for services that our physician reviewers determined were medically necessary.
Nearly half of those enrolled in Medicare are now in Medicare Advantage private for-profit insurance programs instead of Original Medicare.
It is not a trend that is in the interests of patient care.